A physician’s job is to avoid “trial and terror” as one of my senior colleagues taught me early on. Preventing bad implants from reaching the market is vital in orthopaedics. This is especially true since the current implants have a > 95 % 10 year survival. It is therefore great to see Göran Selvik’s RSA method (Selvik et al. 1983) generating headlines in both Acta Orthopaedica and JBJS Am.
In JBJS Am. a valuable 10 year follow-up of 41 hip arthroplasties (Nieuwenhuijse et al. 2012) validate the use of RSA. They could see an impressive correlation between micro motion at 2 years and late follow-up. About one fourth of all the cups turned out to be loose at the end of the follow-up. The C-statistic or area under the receiver operating curve statistic was 0.88 which is close to the ideal 1. The C-statistic is a measure of the specificity (that only the right patients are identified) and sensitivity (that all that later show movement actually are discovered).
I’m surprised by:
- The power they got from only 41 patients. The method has an impressive precision.
- The number of failed components – 1/4. A little more than I would expect with a > 95 % survival rate.
- That components start to loosen already within two years. Is this indicative of surgical technique being the issue?
Nieuwenhuijse, M.J. et al., 2012. Good Diagnostic Performance of Early Migration as a Predictor of Late Aseptic Loosening of Acetabular Cups: Results from Ten Years of Follow-up with Roentgen Stereophotogrammetric Analysis (RSA). The Journal of Bone and Joint Surgery (American), 94(10), pp.874–880.
Selvik, G., Alberius, P. & Aronson, A.S., 1983. A roentgen stereophotogrammetric system. Construction, calibration and technical accuracy. Acta radiologica: diagnosis, 24(4), pp.343–352.
A quick guide to RSA
RSA is an invasive method. You have to during surgery implant tantalum beads (tiny metallic markers) into the skeleton. These beads grow into the bone and become one with the bone. By looking at the different beads in the bone it is therefore possible to get the exact idea of the 3D position of the bone. While the bone has tantalum beads the prosthesis usually has “towers” that stick out and mark the far ends of the implant.
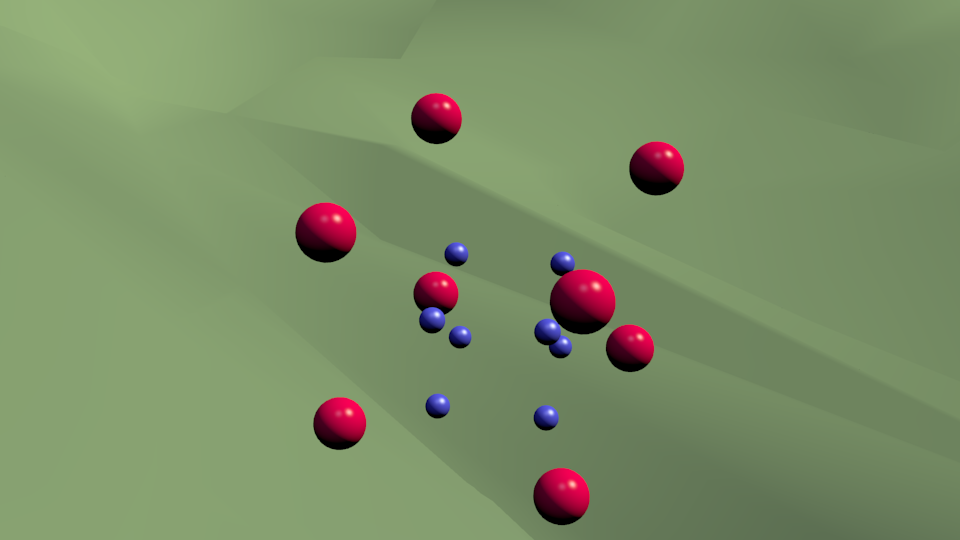
The beeds and the prosthetic gives two 3D objects. I have here a movie showing two boxes in 3D space. The inner blue box would represent the implant and the outer the bone.
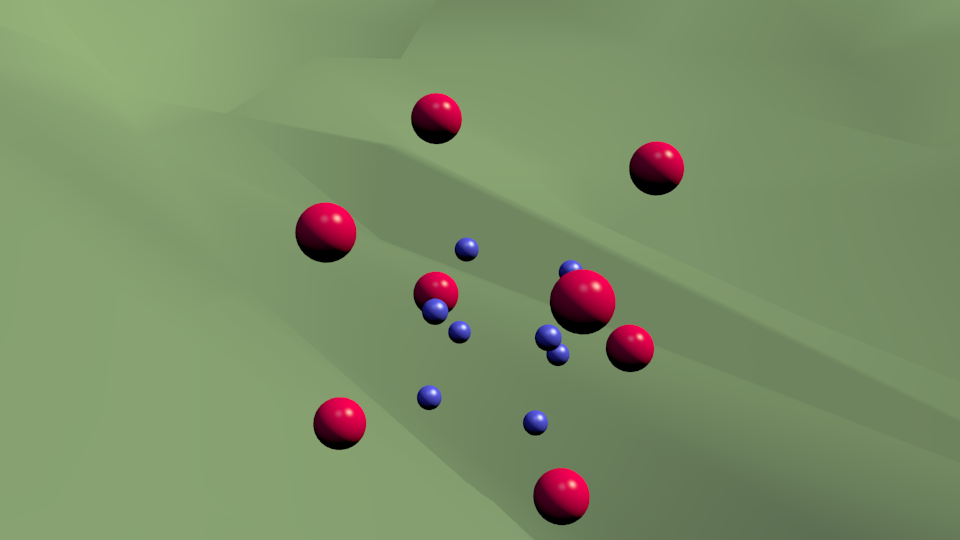
This fancy 3D view is usually not available, what you get looks a little like a still image:
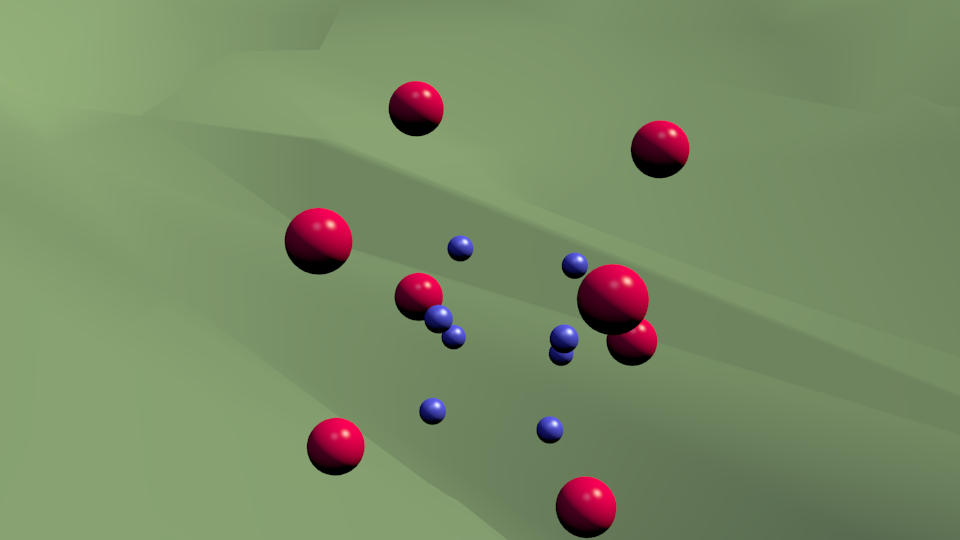
If there is rotation or movement between the elements their relationship slightly changes:
Above you can make out the change but the hard part is that the new image usually has a slightly different angle. This makes it much harder to decide if movement has occurred:
The beauty of Selvik’s method is that the way you get the image doesn’t matter and you get a amazing precision < 1 mm and < 1 degree of rotation!
Images & animation are created with Blender and free for use.