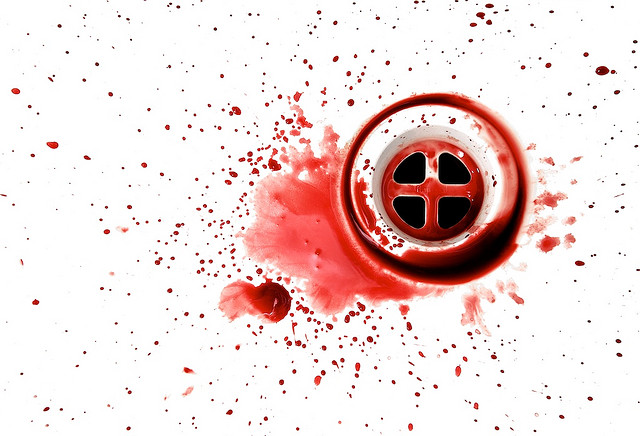
The degenerative cuff tear still unresolved. The image is CC by Brian
I’ve previously reported on Kukkonen et al’s excellent three-armed rotator cuff surgery RCT. They’ve now just published the 2-year follow-up where they still don’t see any difference in outcomes. Interestingly, they’ve added an MRI and noted that the cuff tear remains smaller among those that had surgery. This indicates that the intended surgery works but still too early to see any actual results. Continue reading