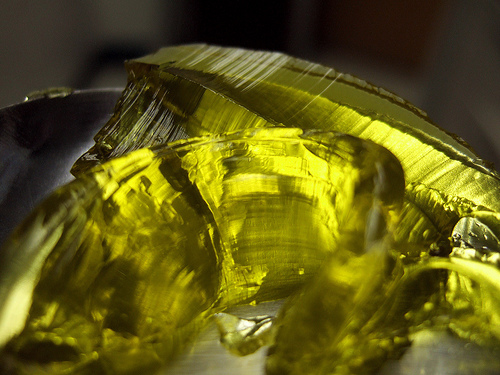
When doing a mosaicplasty you create a mosaic of ostechondral cylinders. These then cover the injury and protect the bone. The picture (cc) is by L D M
Although RCT’s are the golden standard for evaluating techniques, retrospective studies such as Krych et al’s study , “Activity Levels Are Higher After Osteochondral Autograft Transfer Mosaicplasty Than After Microfracture for Articular Cartilage Defects of the Knee: A Retrospective Comparative Study”, can be an interesting read.
They compare microfracturing (se previous post) with mosaicplasty. In mosaicplasty you harvest bone and cartilage cylinders (osteochondral transfer) from sites where it’s not needed and transfer it to the injury. The technique is nice and fairly straightforward although getting all the cylinders aligned perfectly so that none are higher/lower is virtually impossible. It can also be a problem that you don’t have enough unused cartilage to harvest.
The reason why Krych’s study is nice is that they implemented a prospective register in 1999 and have therefore good quality follow-up data. I think it’s really praiseworthy that they started a registry that early. These are rare injuries – it took the team 13 years to get this article published! Continue reading →